Authored By
Andrew Carr and Mark Abraham (DataHaven)
Date
September 09, 2025
Partners
Health Equity Solutions, United Way of Connecticut
The passage of H.R.1, known as the "One Big Beautiful Bill Act," on July 4th, will have major consequences for healthcare coverage in Connecticut. The budget reconciliation bill is projected to cause at least 10 million people to lose their health insurance nationally by 2034, including over one hundred thousand Connecticut residents, according to a new analysis of the bill by KFF. This translates to hundreds, and in many cases thousands, of residents within each town.
"Millions of Americans, including thousands of Connecticut residents, will lose their health insurance because of the [legislation]," said Access Health CT CEO James Michel on July 9. "These changes can be expected to increase costs for customers here in Connecticut, and nationwide, and create barriers to financial help.”
Statewide Impacts: Interactive Maps
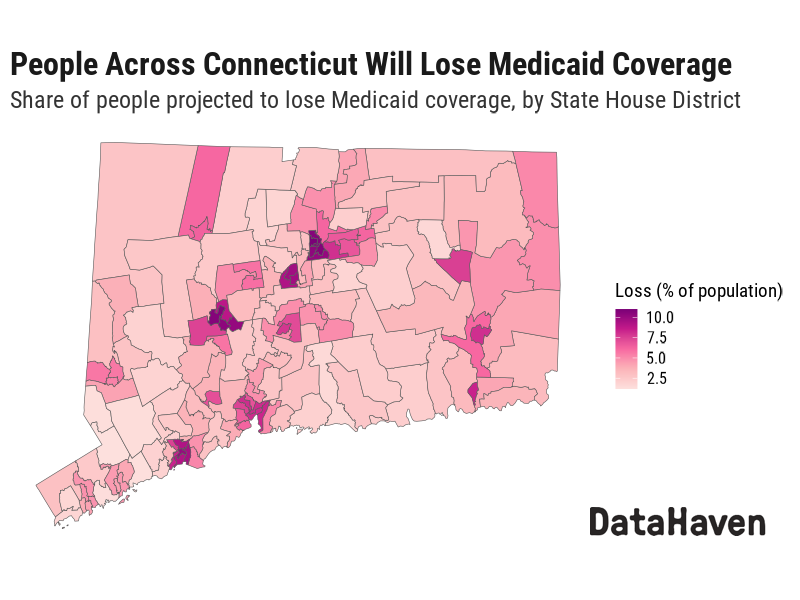
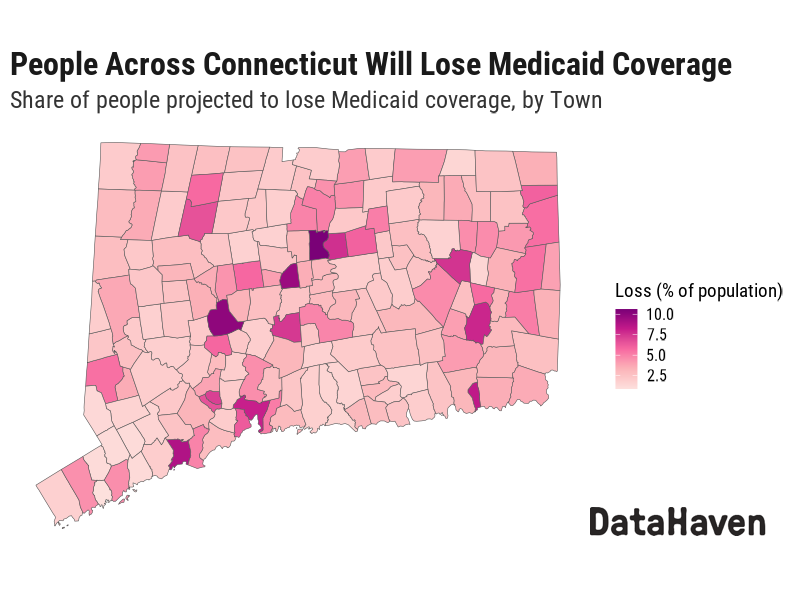
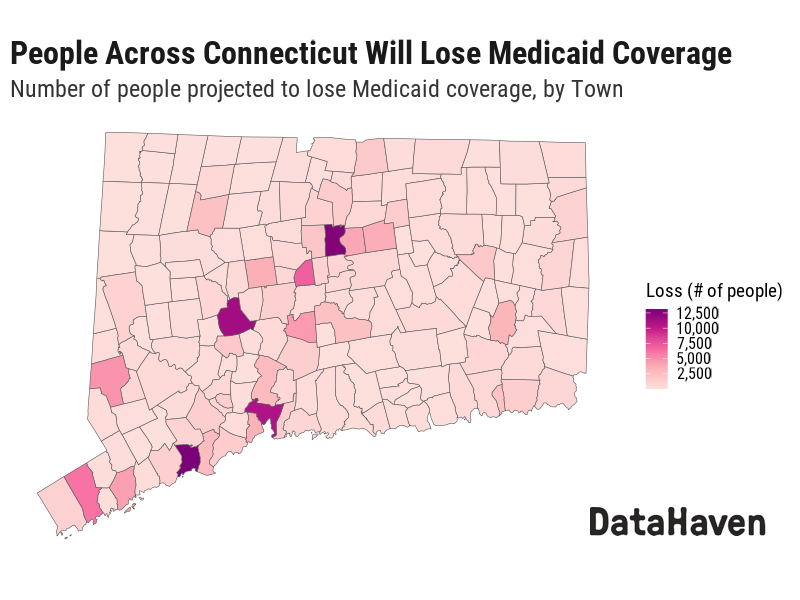
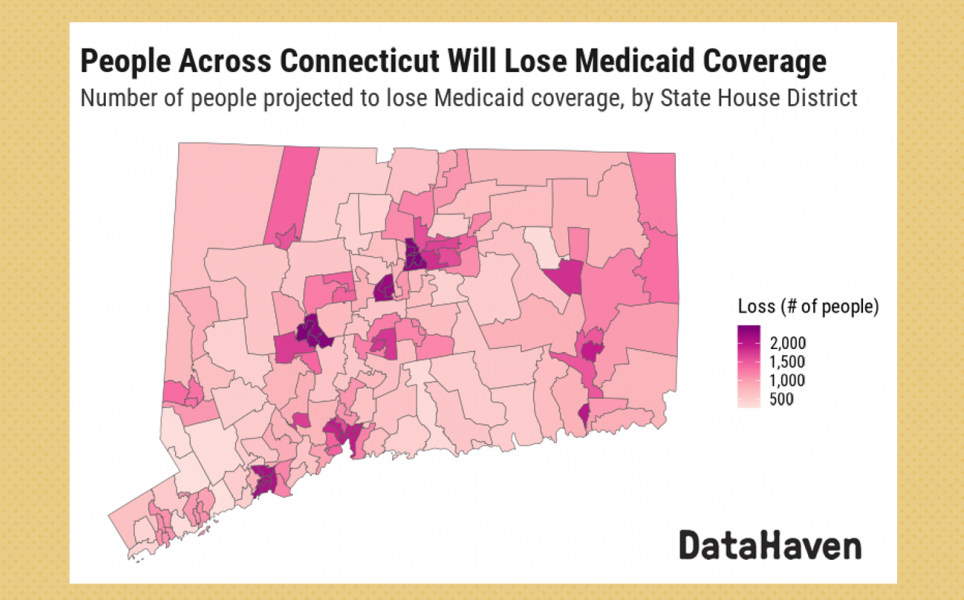
A Medicaid-specific analysis by Manatt estimates that 168,614 people in Connecticut will lose their Medicaid coverage over the next 10 years. The Connecticut Department of Social Services has shared similar estimates.
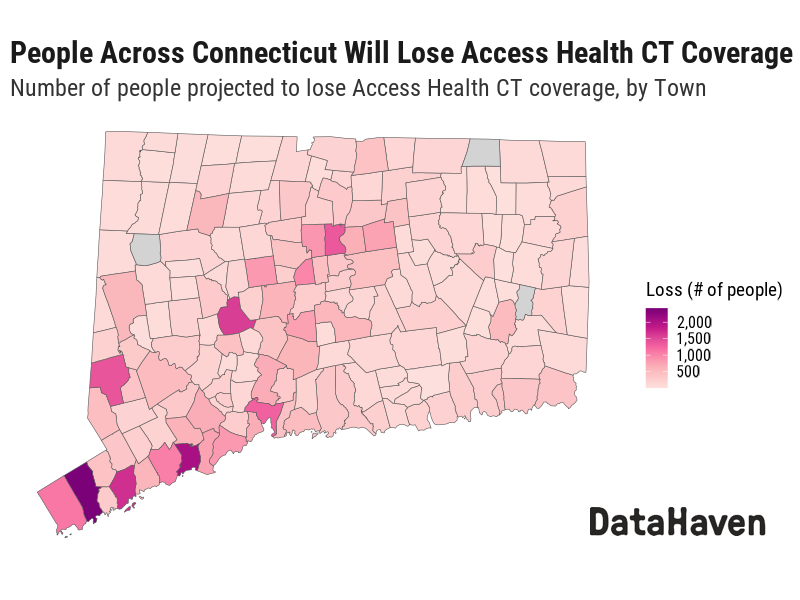
The bill is also projected to have a severe impact on the state's health insurance marketplace, with Access Health CT stating that about one third of their customers, or about 50,000 Connecticut residents, will lose coverage.
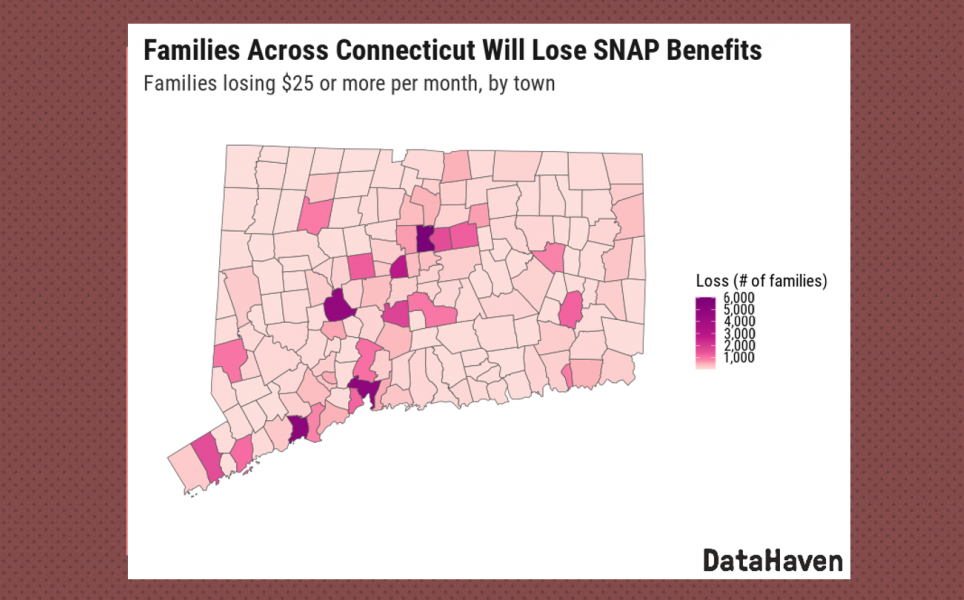
DataHaven used these numbers as a baseline to estimate how many people will lose Medicaid and Access Health CT coverage by town and legislative district throughout Connecticut, as well as by income, race/ethnicity and other characteristics.
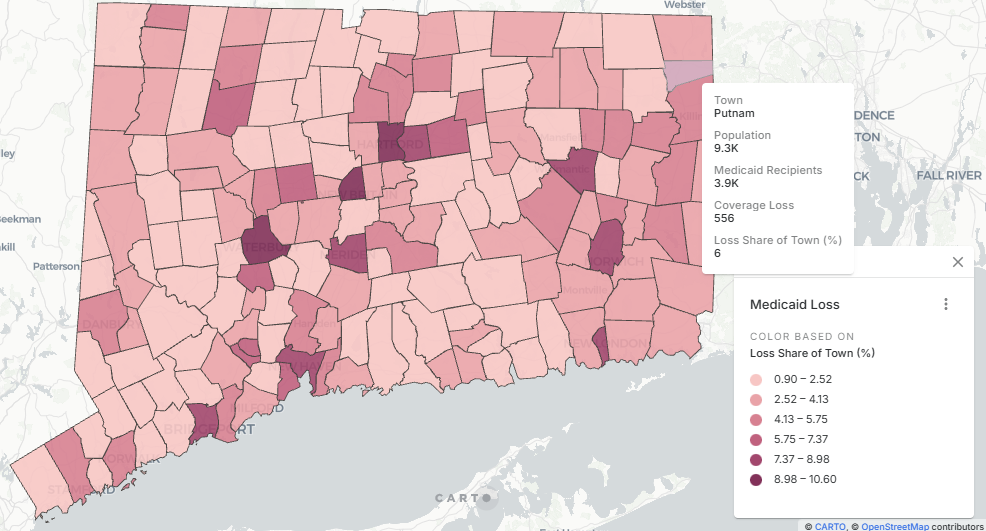
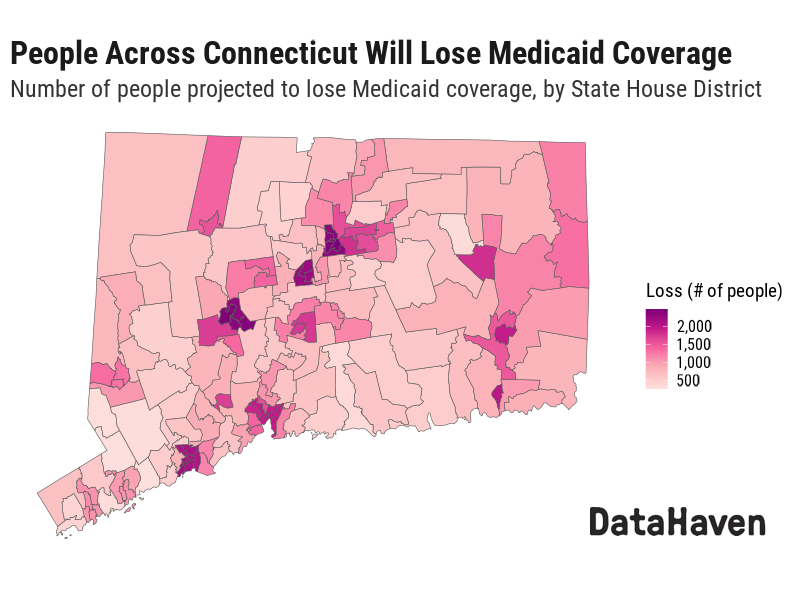
Interactive maps and a spreadsheet with the data are available below. Select a geographic area to see the number with coverage, those projected to lose coverage, and/or the share of total population that would be impacted.
- Share of population projected to lose Medicaid coverage, by town
- People projected to lose Medicaid coverage, by State House District
- People projected to lose Medicaid coverage, by State Senate District
- People projected to lose Access Health CT coverage, by town
Communities Hit Hardest by Medicaid Losses
In Hartford, the new administrative requirements of H.R.1 will cause about 13,000 people to lose Medicaid coverage, which is about 11 percent of that city's entire population. Other towns that will see large losses include Bridgeport (13,000 people), Waterbury (11,000 people), and New Haven (11,000 people).
Coverage losses would have devastating consequences for the entire state, however. For example, in Connecticut's rural State House District 51, which includes parts of Putnam, Killingly, and Thompson, about 1,200 people, or 5 percent of the area's total population, will lose Medicaid coverage. In rural State Senate District 30, which includes most of Litchfield County, 3,800 people, or about 4 percent of that area's total population, will lose coverage. In Torrington, Vernon, and West Hartford, roughly 2,000 people will lose Medicaid in each town, or 7 percent, 5 percent, and 3 percent of the populations of those towns, respectively.
DataHaven used data from the 2019-2023 American Community Survey to estimate the number of people who will lose Medicaid coverage by income, race and ethnicity, household type, and place of birth.
Income Impact
The legislation will hit lower-income residents hardest, with 102,000 Connecticut residents who live below 200 percent of the federal poverty line projected to lose their Medicaid coverage. But many people living within middle-class and "ALICE" households would lose their Medicaid coverage, as well.
Racial and Ethnic Disparities
The legislation is likely to have a major impact on all communities, but also exacerbate racial and ethnic disparities in access to health care. Although non-Hispanic White residents represent the largest absolute number of projected losses (71,000 people, or 3% of the state's White population), communities of color face disproportionate impacts. A total of 56,000 Latino residents (9% of the Latino population) and 27,000 non-Hispanic Black residents (8% of the Black population) are projected to lose coverage. Additionally, 7,000 Asian people and 8,000 people of some other race/ethnicity are projected to lose Medicaid.
Family Structure and Place of Birth
People belonging to a single-parent or other non-married family household are also projected to be disproportionately impacted (71,000 people), although people who are married (62,000 people) will represent over one third of those losing Medicaid.
Finally, the cuts will disproportionately affect people born in the United States, who make up 83.5 percent of the population but 85.2 percent of Medicaid recipients. About 99,000 people who were born in Connecticut and 44,000 people born in other US states, plus 25,000 people born outside the US, are projected to lose Medicaid coverage.
Communities Hit Hardest by Access Health CT Losses
For Access Health CT coverage, the distribution of coverage loss is somewhat different (see interactive maps above). Towns with the largest number of people projected to lose their Access Health CT insurance coverage include:
- Stamford (2,400 people)
- Bridgeport (2,100 people)
- Norwalk (1,700 people)
- Waterbury (1,600 people)
- Danbury (1,400 people)
- Hartford (1,400 people)
- New Haven (1,300 people)
- Greenwich (1,100 people)
- Fairfield (1,000 people)
Again, rural areas are also impacted. For example, in rural Salisbury, Connecticut, about 260 of the town's 4,200 residents are enrolled in Access Health CT, and nearly 100 of those people are projected to lose coverage.
Behind the Coverage Losses
H.R.1 requires that certain adults ages 19 to 64 meet work reporting requirements to be eligible to receive and stay on Medicaid. Specifically, they must demonstrate that they have worked, volunteered, or attended school at least 80 hours per month for up to three consecutive months to maintain coverage. These requirements take effect by January 1, 2027. The administrative burden of meeting these extensive documentation requirements represents the primary driver of expected coverage losses, rather than people's inability to meet the work requirements themselves. The legislation also makes changes to eligibility for immigrant groups. Additionally, H.R.1 lowers the amount that states like Connecticut can tax healthcare providers, which may limit funds available to finance Medicaid, especially considering other changes in the bill such as cuts to SNAP (food stamps).
The legislation is projected to dramatically increase the cost of health insurance enrollment through Access Health CT. First, the bill fails to extend enhanced premium tax credits, which reduce the cost of marketplace health plans in every income bracket. The bill requires other changes to how health insurance marketplaces function including making refugees, people approved for asylum, valid visa holders, and other groups ineligible for certain types of financial help, increasing paperwork requirements and administrative burdens, eliminating special enrollment periods for low-income residents, making changes that could result in fewer covered services, and others that collectively will make it significantly more difficult for residents to enroll or maintain Access Health CT coverage.
These policy changes, more broadly, may result in higher healthcare costs, higher insurance premiums, and/or reduced services for all residents, due to their impact on the types of services that Connecticut hospitals are able to provide if revenues decrease as a result of people losing health insurance as well as other factors.
Policymakers in Connecticut may be able to reduce the negative impacts of these policies, for example, by creating better administrative systems that verify Medicaid eligibility rather than require residents to report their eligibility directly. However, building these systems could take significant time and require large investments.
In addition to this report, DataHaven is including questions related to Medicaid experiences and concerns about loss of other benefits within its 2025 DataHaven Community Wellbeing Survey. Results from that survey will be released later this year.
We hope that residents and policymakers will use the information in this report to help understand the impact that this legislation will have on the place where they live and advocate for improved well-being for all residents.
Report Methods and Acknowledgements
To estimate Medicaid loss in Connecticut towns and districts, DataHaven used an estimate from Manatt Health of the number of people who will lose Medicaid coverage due to H.R.1 over the next 10 years. This was weighted by town-level Medicaid recipients data from the Connecticut Department of Social Services to estimate the number of people projected to lose Medicaid coverage in each town. DataHaven used a town-to-district crosswalk to produce estimates of coverage loss by state legislative district.
Estimates of how many people will lose marketplace health insurance are based on data from Access Health CT on the number of people who have marketplace health insurance by town. A table titled "QHP Enrollment by Town - 081225" was obtained from Access Health CT via email request on August 13, 2025, containing data on current enrollees by "home city," and analyzed by DataHaven to create town-level enrollment estimates. Based on the impact assessment described in the Access Health CT article cited above, these totals were multiplied by one-third to estimate coverage loss over the next 10 years.
We acknowledge Karen Siegel of Health Equity Solutions for their input and feedback on our report methods. A related factsheet is available on the Health Equity Solutions website.
Report Limitations
It is likely that the actual distribution of people losing healthcare coverage as a result of H.R.1 would differ from the estimates in this analysis. However, detailed town-level, address-level, or other personal-level information that could allow DataHaven to produce more precise estimates of coverage loss for each community are not available at this time, and in many cases would be unlikely to be available due to concerns about confidentiality.
As part of this report, DataHaven analyzed additional available public information about the distribution of health insurance coverage types by town and found that using that information would be unlikely to improve the accuracy of these estimates and/or could introduce other sources of error. Residents who have Medicaid or Access Health CT coverage, including those covered by Medicaid expansion, as well as groups such as immigrants, asylees, and lawful permanent residents, often represent a significant share of the population in every community in the state.
Additionally, future changes in state and federal policy could reduce, or increase, the number of people who will lose their health insurance coverage as a result of H.R.1.